Star Health Insurance
India's first standalone health insurer faces scrutiny. Star Health pioneered dedicated health coverage in 2006, but recent IRDAI investigations into claim practices raise questions. With 14,000+ network hospitals and medical inflation at 14-16%, does pioneering status guarantee performance? Let's examine the data behind India's largest standalone health insurer.
Company Overview
Founded in 2006, Star Health and Allied Insurance Company Limited (headquarters: Chennai) holds the distinction of being India's first standalone health insurance provider. IRDAI registration: 129 (dated March 16, 2006). With 31.5% standalone health insurance market share in FY 2024-25, ranking first among SAHIs, serving 32 million lives. Gross Written Premium reached ?16,716 crores with 15% YoY growth. Network encompasses 14,800+ hospitals across 881+ branches and 1,700+ customer touchpoints spanning 25 states and 5 Union Territories. Digital penetration stands at 42% total business.
Product Categories
• Individual Health Plans: ?2 lakh - unlimited coverage
• Family Floater Plans: Shared sum insured up to ?1 crore
• Senior Citizen Plans: Age 60-75 entry, lifelong renewability
• Critical Illness Plans: Lump-sum on diagnosis, ?5 lakh - ?50 lakh
• Super Top-Up Plans: Deductible-based coverage up to ?1 crore
• Maternity Coverage: Available in Comprehensive plans after waiting
• Disease-Specific Plans: Cardiac, cancer, diabetes management programs
• Corporate Group Plans: Employer-sponsored comprehensive policies
General features include hospitalization (24-hour/daycare), pre-post coverage (30-60 days), 600+ daycare procedures, flexible room rent, 100% sum insured reload, NCB up to 50%, AYUSH treatments, ambulance (?2,000). 2026 innovations: Smart Health Pro digital-only product, Super Star Policy modular coverage, AI Face Scan health assessment, telemedicine across 64 cities, home healthcare services, mental health coverage, OPD riders.
Claim Settlement Ratio
Star Health achieved 82.31% CSR for FY 2024-25, below industry average of 89-90%. Three-year trend shows inconsistency: FY 2022-23 at 81.70%, FY 2023-24 at 86.50%, FY 2024-25 at 82.31%—declining performance. Incurred Claim Ratio stands at 66.47%. Practically, out of 100 claims submitted, approximately 82 get settled. This below-average CSR has triggered IRDAI investigations into claim settlement practices, with 2,96,356 claims rejected in FY 2023-24.
Network Hospitals
• Total network: 14,800+ hospitals nationwide
• Delhi-NCR: 420+ hospitals
• Mumbai: 480+ hospitals
• Bangalore: 360+ hospitals
• Chennai: 380+ hospitals
• Hyderabad: 320+ hospitals
• Pune: 290+ hospitals
• Kolkata: 270+ hospitals
• Ahmedabad: 250+ hospitals
Top chains include Apollo, Fortis, Max, Manipal, Medanta, Narayana Health, Columbia Asia, Cloudnine. Tier 2/3 cities like Jaipur, Lucknow, Indore, Coimbatore, Visakhapatnam comprehensively covered. Cashless approval: planned admissions 2-4 hours, emergency 24 hours claim settlement. Reimbursement processes within 30 days (no investigation), 45 days (with investigation). Complaint ratio: 52.31 per 10,000 claims (FY 2024-25)—significantly higher than industry peers averaging below 20.
Tax Benefits (Section 80D)
• Self/spouse/children (below 60): ?25,000
• Self/spouse/children (60+): ?50,000
• Parents (below 60): ?25,000 additional
• Parents (60+): ?50,000 additional
• Preventive check-ups: ?5,000 (within limits)
• Maximum deduction: ?1,00,000/year
A 35-year-old professional covering senior parents paying ?70,000 annual premium claims ?75,000 deduction (?25,000 self + ?50,000 parents), saving ?23,250 at 31% bracket—substantially offsetting premium costs.
Portability & Claim Rejection Prevention
Portability: Transfer to Star Health while retaining waiting period credits from previous insurer. Submit portability application 45-60 days before current policy expiry, provide existing policy documents, Star Health verifies transfer request, underwriting conducted if coverage increases, seamless transition maintains continuous coverage. Completed waiting periods (pre-existing conditions, specific illnesses) automatically transfer.
Claim Rejection Prevention:
• Non-disclosure: Truthfully declare all pre-existing conditions during purchase
• Waiting periods: Verify completion before scheduling elective procedures
• Exclusions: Thoroughly review policy document exclusion clauses
• Documentation: Maintain complete hospital bills, discharge summaries, reports
• Intimation: Notify insurer within 24 hours emergency hospitalization
• Network: Use network hospitals ensuring guaranteed cashless facility
Exclusions, Support & Recommendation
Waiting Periods:
• Initial: 30 days (accidents covered day-one)
• Pre-existing diseases: 3-4 years standard
• Specific diseases: 2 years (hernias, cataracts, joint replacements)
• Maternity: 36 months
Note: Portability credits transfer completed waiting periods seamlessly.
Permanent Exclusions: Cosmetic procedures except accident reconstruction, dental treatments unless accident-related, eyeglasses and hearing aids, self-inflicted injuries, substance abuse complications, experimental treatments, congenital diseases in standard plans, infertility treatments without specific riders.
Customer Support: 24/7 helpline (1800-425-2255), mobile app with e-card access, AI Face Scan, hospital locator, claim tracking, email support, WhatsApp assistance, 881+ physical branches, 1,700+ customer touchpoints nationwide. Grievance escalation: IRDAI IGMS portal, Insurance Ombudsman resolution.
Why Choose & CTA: Star Health offers India's first SAHI status, largest 14,800+ hospital network, 31.5% market leadership, innovative AI Face Scan tool, telemedicine across 64 cities, unlimited coverage options. Honest limitations: below-average 82.31% CSR, IRDAI investigations ongoing, elevated 52.31 complaint ratio, 2.96 lakh claims rejected annually. Compare policies free at NiveshKaro.com—IRDAI-certified advisors, zero commission, instant quotes!
Disclaimer: NiveshKaro.com offers free guidance via IRDAI advisors—zero commission. Data accurate as of January 2026, subject to change. Verify terms with Star Health and Allied Insurance Company Limited. Visit niveshkaro.com today.
Expert Calling
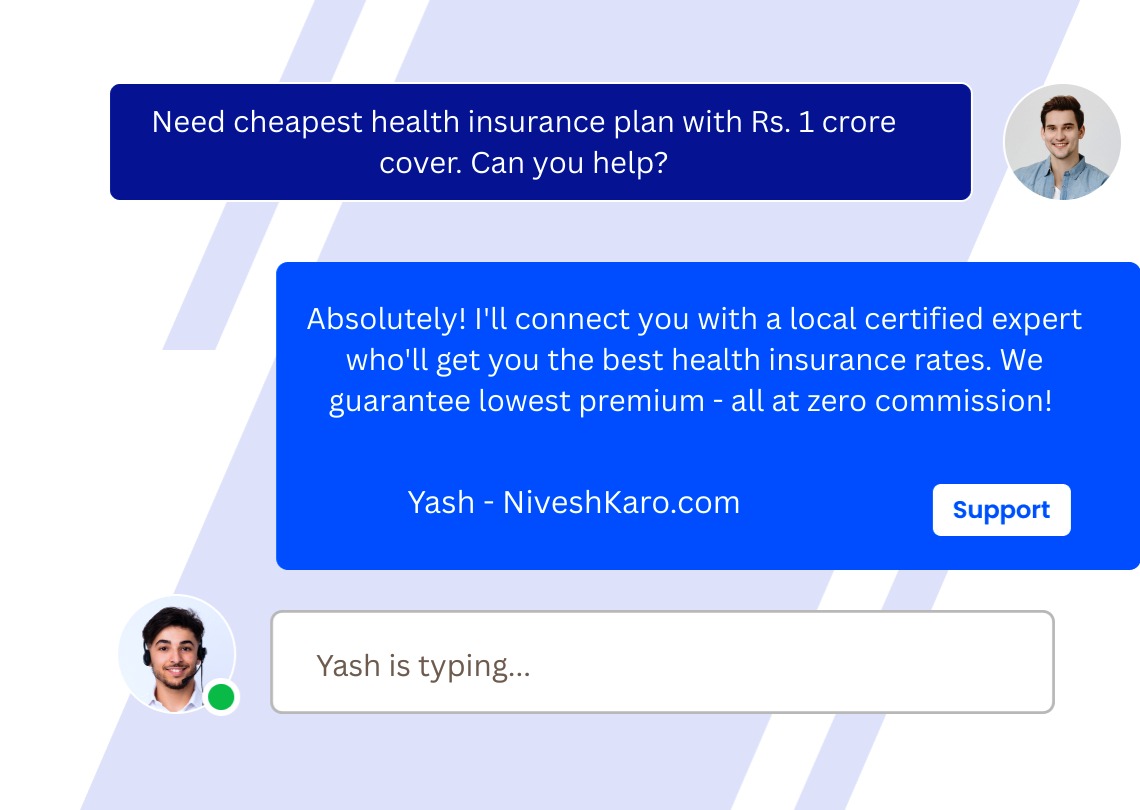
Always Available Support
Real-Time Support When
You Need It
Our expert support team connects you with certified local financial advisors for life insurance, health insurance, car insurance, bike insurance, mutual funds, SIP investments, tax planning, retirement planning, and wealth management services — all at absolutely zero cost with guaranteed best deals.
Instant Call Connect
Submit your information — we call you back within minutes guaranteed.
Call Back Service
Schedule your call — speak with local consultants at your preferred timing.